
1.1 History
You are here: GCP training > Menu > Training Package > History
 |
|||
|
1.1 History |
|||
|
This
Unit reviews significant historical events that have influenced current
ethical guidelines and national and international regulations; the fundamental
ethical principles that guide the ethical conduct of research involving
human participants; and the role of international guidelines in the
protection of human participants. SIGNIFICANT HISTORICAL EVENTS 1.
Nazi Medical War Crimes Although not the first example of harmful research on unwilling human participants, the experiments conducted by the Nazi physicians during World War II were unprecedented in their scope and the degree of harm and suffering to which human beings were subjected. The "medical experiments" were performed on thousands of concentration camp prisoners and included such deadly studies as injecting people with gasoline and live viruses, immersion in ice water, and forcing people to ingest poisons. In
December 1946, 23 physicians and administrators, many of them leading
members of the German medical hierarchy, were indicted before the war
crimes tribunal at Nuremberg for their willing participation in the
systematic torture, mutilation, and killing of the prisoners in experiments.
Despite the arguments of the German physicians that the experiments
were medically justified, the Nuremberg Military Tribunals condemned
the experiments as "crimes against humanity"; 16 of the 23
physicians were found guilty and imprisoned, and 7 were sentenced to
death. In the August 1947 verdict, the judges included a section called
"Permissible Medical Experiments." This section became known
as the Nuremberg Code and has formed the basis for ethics codes internationally.
2. The Tuskegee Syphilis Study The most notorious example in the United States of prolonged and knowing violations of the rights of a vulnerable group of research participants was the long-term study of black males conducted at Tuskegee by the United States Public Health Service. This study was initiated in the 1930s as a study of the natural history of untreated syphilis and continued until 1972. Over 400 black men with syphilis participated and about 200 men without syphilis served as controls. The men were recruited without informed consent and, in fact, were misinformed that some of the procedures done in the interests of research (e.g., spinal taps) were actually "special free treatment." By 1936, it was apparent that many more infected men than controls had developed complications and, ten years later, a report of the study indicated that the death rate among those with syphilis was about twice as high as it was among the controls. In the 1940s, penicillin was found to be effective in the treatment of syphilis. The study continued, however, and the men were neither informed nor treated with the antibiotic. The first accounts of this study appeared in the national press in 1972. The resulting public outrage led to the appointment of an ad hoc advisory panel by the Department of Health, Education and Welfare to review the study and give advice on how to assure that such experiments would never again be conducted. Among the recommendations was the request that Congress establish a "permanent body with the authority to regulate, at least, all federally-supported research involving human subjects." In acknowledgement of its responsibility, the government continues to compensate the surviving participants and the families of deceased participants. 3.
The Jewish Chronic Disease Hospital Study In 1963, studies were undertaken at New York's Jewish Chronic Disease Hospital to understand whether the body's inability to reject cancer cells was due to cancer or debilitation. Previous studies had indicated that healthy persons reject cancer cells promptly and the researchers allegedly believed that the debilitated patients would also reject the cancers but at a substantially slower rate when compared to healthy participants. These studies involved the injection of foreign, live cancer cells into patients who were hospitalized with various chronic debilitating diseases. The consent had been given orally, but did not include a discussion on the injection of cancer cells, and a consent was not documented. The researchers felt that documentation was unnecessary because it was customary to undertake much more dangerous medical procedures without the use of consent forms. Further, patients were not told that they would receive cancer cells because the researchers felt it would unnecessarily frighten the patients. Researchers defended this view on the basis that they had good cause to predict that the cancer cells were going to be rejected. In subsequent review proceedings conducted by the Board of Regents of the State University of New York, it was found that the study had not been presented to the hospital's research committee and that the several physicians responsible for the patients' care had not been consulted. The researchers were found guilty of fraud, deceit and unprofessional conduct. 4. The Willowbrook Study The vulnerability of children, especially institutionalized children, as participants in research is demonstrated in a series of studies conducted from 1963 through 1966 at the Willowbrook State School, a New York institution for "mentally defective" children. In order to gain an understanding of the natural history of infectious hepatitis under controlled circumstances, newly-admitted children were deliberately infected with the hepatitis virus. Researchers defended the deliberate injection of these children by pointing out that the vast majority of them acquired the infection anyway while at Willowbrook, given the crowded and unsanitary conditions, and because only children whose parents had given consent were included. During the course of these studies, Willowbrook closed its doors to new patients, claiming overcrowded conditions. However, the hepatitis program, because it occupied its own space at the institution, was able to continue to admit new patients. Thus, in some cases, parents found they were unable to admit their child to Willowbrook unless they agreed to his or her participation in the studies. This controversial case raised important questions about the adequacy and freedom of consent, inadequate disclosure of the child's risk of later developing chronic liver disease, and the lack of information given to parents about access to doses of gamma-globulin for other children. |
|||
|
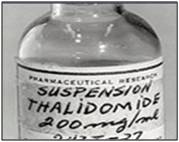
5. Thalidomide
|
 |
||

BACK TO MENU |
 |